Pain is something everyone experiences, but many of the things we believe about it are flat-out wrong. These misconceptions can make pain worse, delay recovery, and even lead to harmful treatment choices. For example, some people think that all pain means a serious injury, while others assume opioids are the only solution. Neither is true.
In this guide, we’ll bust six of the most common pain myths, explain what science really says, and share healthier strategies to manage pain effectively.
Myth #1: Pain Always Means a Serious Injury
One of the biggest misconceptions is that pain always equals serious damage. While pain can be a warning sign, it doesn’t automatically mean you’re badly injured.
How Your Nervous System Plays a Role
Your nervous system acts like an alarm system. Sometimes, it gets overly sensitive and amplifies pain signals, even when the actual injury is minor—or in some cases, when there’s no tissue damage at all.
- Conditions like fibromyalgia and chronic pain syndromes often involve this kind of “overactive alarm system.”
- This is why two people with the same injury may feel pain very differently.
Acute vs. Chronic Pain
- Acute pain: Short-term, caused by an injury, surgery, or illness. It usually improves as you heal.
- Chronic pain: Lasts for weeks, months, or years—even after the body has healed. It can exist without an obvious injury.
👉 Takeaway: Pain is complex. Not all pain means something is “broken.” Understanding this helps people avoid unnecessary fear and treatments.
Myth #2: Rest is the Best Way to Heal
It’s natural to want to lie down when you’re hurting, but too much rest can backfire.

Why Movement Matters
Research shows that gentle activity helps recovery by:
- Boosting blood flow → delivering oxygen and nutrients to tissues.
- Reducing stiffness → keeping joints flexible and muscles strong.
- Maintaining mobility → preventing long-term weakness.
For example, people recovering from low back pain often do better with gentle movement (like walking or stretching) than complete bed rest. Source: Harvard Health.
Finding the Right Balance
The best approach is “relative rest”—avoiding activities that make pain worse but staying as active as possible.
- Try low-impact exercises like swimming, yoga, or light walking.
- A physical therapist can design a plan tailored to your condition.
👉 Takeaway: Rest isn’t always best. Movement, when done safely, speeds recovery.g.
Also Read: What are Safe Natural Remedies for Arthritis Pain?
Myth #3: Pain is Inevitable as We Age
A lot of people believe that pain is just part of getting older. While it’s true that aging can bring changes to Yes, our bodies change with age. But pain doesn’t have to be part of the package. Many older adults live full, active lives without constant pain.

How Lifestyle Choices Affect Pain
Factors that play a huge role in pain prevention:
- Diet → Eating anti-inflammatory foods (like leafy greens, berries, and fatty fish) lowers the risk of arthritis flare-ups.
- Exercise → Strength training and stretching keep joints healthy.
- Stress management → Mindfulness, yoga, and relaxation techniques reduce stress-related pain.
- Sleep quality → Poor sleep increases pain sensitivity.
How to Age Without Pain
- Get regular health checkups.
- Maintain a healthy weight to reduce pressure on joints.
- Stay active with low-impact exercises like cycling or water aerobics.
- Seek professional help early if pain persists.
👉 Takeaway: Aging doesn’t guarantee pain—you have more control than you think.
Also Read: What Practices Aid Recovery After a Sprain?
Myth #4: Opioids Are the Only Answer for Severe Pain
Opioids can help in some cases, but they’re not the only option—and not always the safest one.

The Dangers of Opioids
- High risk of addiction and dependence.
- Over time, people may need higher doses for the same relief.
- Side effects include constipation, drowsiness, and breathing problems.
- The U.S. opioid crisis shows the dangers of over-reliance. Source: CDC.
Better Ways to Manage Pain
A multimodal approach often works best:
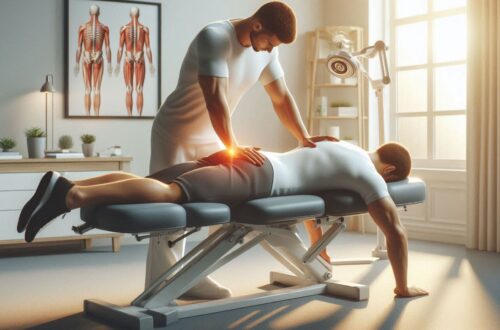
- Physical therapy → Builds strength and reduces stiffness.
- Non-opioid meds → Ibuprofen, acetaminophen, or prescription alternatives like gabapentin.
- Interventional procedures → Nerve blocks or injections.
- Psychological therapies → CBT helps patients reframe how they cope with pain.
- Complementary therapies → Acupuncture, massage, and meditation.
👉 Takeaway: Opioids are just one tool—not the only one. Safer, long-term strategies often work better.se options, people can often manage their pain effectively while avoiding the risks of opioids. A pain specialist can help create a personalized plan tailored to your needs.
Myth #5: If Pain Comes and Goes, It’s Not Serious
Intermittent pain is easy to dismiss, but recurring pain shouldn’t be ignored.

Understanding Chronic Pain
Chronic pain often flares up and eases off. That doesn’t mean the problem is gone. Conditions like arthritis, migraines, or nerve pain can wax and wane.
Why You Shouldn’t Ignore Recurring Pain
- Early treatment prevents worsening.
- Doctors can identify hidden causes before they escalate.
- Managing pain early improves your quality of life.
👉 Takeaway: Don’t wait until the pain becomes unbearable. If it keeps coming back, get it checked.e.
Also Read: How do I Choose an Ergonomic Chair for Lower Back Support?
Myth #6: Pain is Just in Your Head
The phrase “it’s all in your head” is dismissive and harmful. While thoughts and emotions influence pain, that doesn’t mean pain isn’t real.

The Mind-Body Connection
- Stress intensifies pain signals.
- Anxiety and depression make pain worse, while pain can also trigger these conditions.
- Coping strategies like mindfulness or therapy change how pain feels.
A Holistic Approach to Pain
Effective pain management often combines physical and mental care:
- CBT (Cognitive-Behavioral Therapy) → Teaches coping strategies.
- Mindfulness meditation → Calms the nervous system.
- Support groups → Provide emotional encouragement.
👉 Takeaway: Pain is both physical and emotional. Treating both aspects gives better results.
Myth #6: Pain is Just in Your Head
The phrase “it’s all in your head” is dismissive and harmful. While thoughts and emotions influence pain, that doesn’t mean pain isn’t real.
The Mind-Body Connection
- Stress intensifies pain signals.
- Anxiety and depression make pain worse, while pain can also trigger these conditions.
- Coping strategies like mindfulness or therapy change how pain feels.
A Holistic Approach to Pain
Effective pain management often combines physical and mental care:
- CBT (Cognitive-Behavioral Therapy) → Teaches coping strategies.
- Mindfulness meditation → Calms the nervous system.
- Support groups → Provide emotional encouragement.
👉 Takeaway: Pain is both physical and emotional. Treating both aspects gives better results.
Conclusion: Rethinking Pain Management
Pain is not always what it seems. Believing the wrong myths—like “pain always means injury” or “opioids are the only solution”—can keep people stuck in cycles of suffering.
By understanding how pain really works and exploring safer, holistic strategies, you can:
- Heal faster.
- Reduce stress around pain.
- Take back control of your life.
If pain keeps interfering with your daily activities, don’t ignore it. Seek professional help—there are more options than you think.
FAQs About Pain Myths
Q1. Can pain exist without an injury?
Yes. Chronic pain conditions like fibromyalgia or nerve pain often occur without clear tissue damage.
Q2. Should I avoid all exercise when I’m in pain?
Not necessarily. Gentle movement often speeds recovery. A doctor or physical therapist can guide you.
Q3. Do older people have to live with pain?
No. With healthy lifestyle choices, many seniors enjoy active, pain-free lives.
Q4. Are opioids safe for long-term pain management?
Generally no. Long-term use carries high risks of addiction and side effects. Other options are safer.
Q5. How do emotions affect pain?
Stress, anxiety, and depression can make pain feel worse. Mind-body techniques like meditation can help.
 Skip to content
Skip to content