Before making any lifestyle changes, it’s always helpful to understand why those changes matter. When you know the “why,” it’s easier to stay motivated and see if the effort is worth it—especially when it comes to diet.
Food, like many rewarding things in life, can be addictive. It directly affects dopamine levels, the brain’s pleasure chemical, which influences motivation and impulsivity. Early research even suggests that dopamine plays a role in diet-induced obesity.
So, what does this have to do with chronic pain? A lot.
Nutrition is all about how your body processes the food you eat. The way you fuel your body can either help you heal or contribute to illness and disease. In this section, we’ll explore how nutrition impacts chronic pain, how lifestyle choices affect food metabolism, and why making changes to your diet can be a powerful step toward better health.
The information here is backed by research from the past decade, providing clear evidence on why shifting your diet and lifestyle can make a real difference for those living with chronic pain.
Chronic Pain: More Than Just Medication
A 2019 article, The Landscape of Chronic Pain: Broader Perspectives, dives into the complexity of chronic pain and its management. It points out that dealing with chronic pain isn’t just about taking medication and seeing doctors—it’s about addressing all aspects of life.

Modern pain management now includes social prescribing, which encourages meaningful social interaction to improve well-being. It also highlights how unhealthy lifestyle choices—like being sedentary, eating poorly, smoking, dealing with anxiety and depression, and even lack of sunlight—can make chronic pain worse.
The Whole-Person Approach to Pain Management
Another study, Time to Flip the Pain Curriculum? (2013), stresses the importance of looking at pain from all angles, not just the medical side. A person’s mental, emotional, and social well-being play a huge role in their pain experience.
The study even used brain scans (fMRI) to show how lifestyle factors impact brain activity, which in turn influences pain perception. This reinforces the idea that treating chronic pain isn’t just about pills—it’s about treating the whole person.
How Diet Plays a Role in Preventing Disease
A massive study published in The Lancet in 2017 analyzed diet-related health risks in 195 countries. The findings?

- High sodium intake,
- Low whole-grain consumption, and
- Low fruit intake
…were among the biggest dietary risk factors for non-communicable diseases.
Shockingly, poor diet was linked to 50% of deaths and 66% of disability-adjusted life years (DALYs). In other words, eating better could prevent 1 in 5 deaths worldwide.
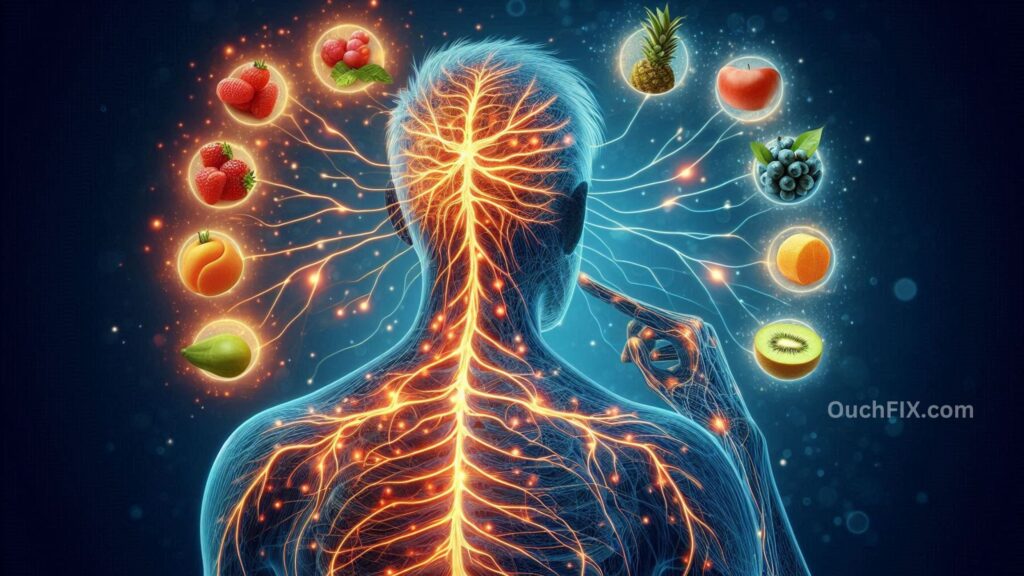
Can Nutrition Help Reduce Chronic Pain?
A 2019 study, Nutritional Intervention in Chronic Pain, found that inflammation in the nervous system plays a key role in chronic pain. And what fuels inflammation? Diet.
The research suggests that a low-saturated fat, low-added sugar diet may:
- Reduce oxidative stress (which damages cells),
- Prevent inflammation from spreading to the brain (a trigger for chronic pain), and
- Improve gut health, which is increasingly linked to pain management.
Also Read: What Common Misconceptions About Pain Management do Experts Highlight?
Personalized Nutrition for Pain Management
A 2016 study, Combining Pain Therapy with Lifestyle, looked at the connection between pain, diet, and lifestyle. It found that fighting obesity, exercising, and personalizing nutrition can improve pain outcomes.

Some promising dietary choices for pain relief include:
- Omega-3 fatty acids (found in fish and flaxseeds),
- Curcumin (the active compound in turmeric),
- Polyphenols (powerful antioxidants found in Mediterranean foods like berries, olive oil, and dark chocolate).
The Role of Diet in Inflammation and Chronic Disease
Another study, Dietary Polyphenols and Chronic Disease Prevention (2019), examined how low-grade, long-term inflammation (metainflammation) contributes to conditions like diabetes, heart disease, and neurodegenerative disorders.
Common dietary patterns that fuel inflammation include:
- Eating too many processed and high-glycemic foods,
- Consuming too little fiber, omega-3s, and healthy fats,
- Eating too much sodium and red meat.
But the study found that polyphenols—abundant in plant-based foods—may help slow down the progression of chronic diseases by reducing oxidative stress and inflammation.
A Whole-Person Approach to Chronic Pain
Another study, Understanding Chronic Pain in a Lifestyle Context, highlights how chronic pain isn’t just physical—it’s influenced by lifestyle. It found that metainflammation can affect the nervous system, triggering the release of chemicals that keep pain signals firing.
The key takeaways?
- Chronic pain is linked to lifestyle choices like exercise, diet, sleep, stress, and even past trauma.
- A “whole-person” approach—combining nutrition, physical activity, and mental health support—may help reduce chronic pain.
Nutrition and Aging: Preventing Pain-Related Disability
A 2020 study, Nutrients and Chronic Pain in Aging, explored how diet affects muscle and joint pain in older adults. The findings suggest that proper nutrition can help maintain mobility and reduce pain-related disability.
Nutritional strategies found to be beneficial include:
- Eating more fish, soy, and eggs,
- Taking magnesium, vitamin D, and omega-3 supplements,
- Adding curcumin and gingerol (anti-inflammatory compounds found in turmeric and ginger).

Also Read: What Advice is Available for Managing Pain Without Medication?
The Link Between Diet and Pain Sensitivity
A 2020 study, Do Nutritional Factors Interact with Chronic Musculoskeletal Pain?, reviewed the impact of different diets on pain.
- Vegetarian and vegan diets may help reduce chronic musculoskeletal pain.
- Weight-loss diets may decrease pain in osteoarthritis.
- High-sugar, high-fat, and high-protein diets were associated with higher pain intensity.
- The Mediterranean diet, known for its anti-inflammatory properties, may help relieve pain.
The study also highlighted how gut health plays a major role in pain. Plant-based diets help maintain a healthy gut microbiome, which can reduce overall inflammation and pain sensitivity.
Final Thoughts
The science is clear: what you eat affects your pain levels. Chronic pain isn’t just a medical condition—it’s influenced by diet, lifestyle, and mental well-being.
By making small but meaningful changes—like incorporating anti-inflammatory foods, maintaining a healthy weight, and managing stress—you can take an active role in managing chronic pain.
Even small steps, like swapping processed foods for whole foods or adding more fruits and veggies to your diet, can make a big difference in how you feel over time.